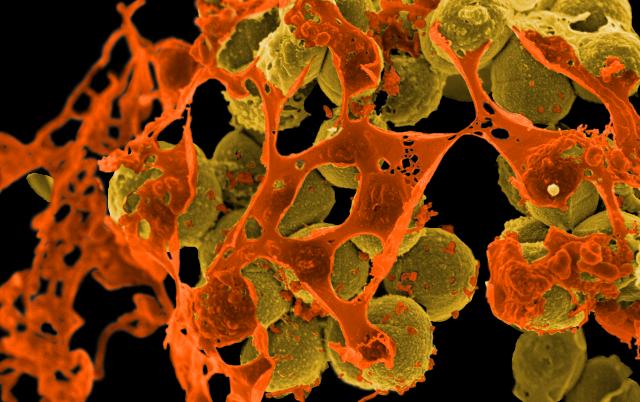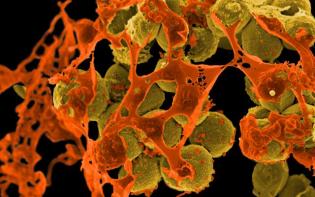
Methicillin-resistant Staphylococcus aureus (MRSA). (Photo by the National Institute of Allergy and Infectious Diseases.)
A few weeks back, we reported on a study out of the University of Iowa that tested supermarket pork for antibiotic-resistant Staph bacteria (aka MRSA). The researchers found MRSA at the same rate for conventionally raised meat and for meat raised without antibiotics. In her well-respected WIRED blog on the topic, Superbug, Maryn Mckenna summed up the media response to the news like this:
There’s just as much resistant bacteria on drug-free meat as there is on conventional meat, so why spend the money — or raise the alarm over farm antibiotic use?
But she disputed that conclusion:
My takeaway is that, in its underlying data, the study proves what campaigners against ag antibiotic use keep saying: that once you use antibiotics indiscriminately and drive the emergence of resistant organisms, you have no way of predicting where that resistance DNA will end up.
For most of us, any sign of MRSA in our food is pretty creepy. (Although the bacteria doesn’t make it through the cooking process, meat can still be what scientists call a “vector,” or a mode of transmission, when we handle it). So we tracked down McKenna, who is also a columnist and contributing editor for Scientific American and the author of Superbug: The Fatal Menace of MRSA. Her take on the research may surprise you.
Q. What should we know about this latest MRSA study?
A. This study was done by the only research team in the U.S. investigating the occurrence of what people call “livestock-associated MRSA.”
[Note: Livestock-associated MRSA is the term for MRSA that was recently discovered to have spread from farm animals to humans. Most MRSA is human-associated, i.e. it arose in hospitals and elsewhere in communities. The study also found this more common type of MRSA on the meat, especially in the stuff raised without antibiotics. McKenna will say more about why this matters below.]

Maryn McKenna.
This is the group that identified it in pigs and farmworkers in Iowa and Illinois in 2009. Since they’re the only ones keeping track of this, to my mind, anything they do is interesting.
This study also represents the largest attempt to sample retail meat in the U.S. for livestock MRSA. What the paper ends up finding is that there is MRSA on meat, but most of it is not the livestock kind.
Also, there are similar amounts of MRSA on meat that is conventionally raised in confinement agriculture [Concentrated Animal Feeding Operations, or CAFOs] and meat that is raised without antibiotics. That result is what led people to say, “Why are we saying this is such a big problem?”
[However,] if you really drill down into its findings, you can in fact see a ton of influences from farm antibiotic use. If you look into their results what you find is that an awful lot of the MRSA they found (both livestock-associated and human-associated on both kinds of meat) actually shows influence of farm antibiotic use. That makes this paper more important than anybody realized.
Q. Well, that’s certainly not what you’d expect from the media reaction to the paper. How did you reach that conclusion?
A. There is one particular type of resistance found by the researchers that is a big red flag for the influence of farm antibiotics, and that is resistance to the antibiotic tetracycline.
Let’s back up. When someone gets an infection, you give them a drug. Maybe it’s not the right dosage and the bacteria become more resistant to that drug. If the bacteria are never exposed to the drug, it’s unlikely they’ll become resistant.
Yet lots and lots of the bacteria that were analyzed in this study were resistant to tetracycline. And doctors haven’t historically given tetracycline to humans with MRSA infections. It’s not one of the major drugs. But animals get lots of tetracycline. The MRSA strain in livestock that was first identified back in 2004 that went from pigs to humans was tetracycline-resistant. In fact, that form of resistance was a big arrow pointing back to the drugs given to the pigs.
And indeed, when you look at all the bacteria samples that the Iowa team analyzed you see tetracycline resistance in lots of them. [Whereas] the human strains of MRSA found on the meat were probably put there by a slaughterhouse worker or a butcher or someone handling it in the supermarket.
These results turn this paper on its head. What it says is not, “Oh, farm antibiotics aren’t having that big an effect.” The prevalence of tetracycline resistance in all forms of MRSA tell us that farm antibiotics are a much bigger deal than anybody realized.
Q. Let’s jump to the way that it was covered in the media, including at Grist but also at the journal Science. People seemed quick to assume that MRSA was found in organic pork. Why the confusion?
A. In the study, the meat raised without antibiotics was from farms that do not use growth promoter or prophylactic antibiotics, but they are not USDA Certified Organic farms. I think people don’t understand the difference.
Q. We also need to recognize that organic isn’t necessarily off the hook either in terms of MRSA contamination on retail meat.
A. Right. But the issue with farm use of antibiotics is not just that resistant organisms end up on meat. That is a concern but it’s not the only concern.
Once you stimulate the emergence of resistant organisms by using antibiotics in inappropriate ways on farms, some percentage of those organisms — exactly how much we don’t know because we’re not allowed to measure on farms — end up in the farms’ manure lagoons. And then they blow off in dust or get into wastewater or otherwise end up in the environment of the farm.
From there they get carried off by the farmworkers or they infect [other] workers. Those organisms then go all over the place. In the wake of this study, people were saying, “Since as much resistant bacteria is on meat without antibiotics, the whole concern about antibiotic use on farms is misplaced.” That’s only true if you think that retail meat is the only place where the resistant organisms show up. But it’s not.
Q. You also found an interesting detail regarding the source of the MRSA-positive meat that was raised without antibiotics.
A. Every “raised without antibiotics” sample that had a positive result for human MRSA came from one [New York area] market. It’s not a flaw in the methodology of the paper but it’s an interesting result.
So, all those human strains on alternative meat turned out to come from the same market and the same chain. It’s a pointer to where they need to go next if they want to continue this research. You have to figure out to what degree contamination with human strains is actually coming from humans. The human strains could get on to meat because a single worker puts it there.
But there’s also the slaughter component. Are slaughterhouses slaughtering both conventionally raised and alternatively raised meat and to what degree are they cleaning and disinfecting their equipment and personnel between the two? The next step is to figure out what the real avenues of contamination are.
Q. In the end, what are the implications for the consumer?
A. There are a couple of different implications. The first is that it tells us livestock-associated MRSA is out there in the environment. That’s important because there haven’t actually been very many papers that found that.
The second point is that there are antibiotic-resistant organisms on raw meat. And that is a concern because, even though MRSA is killed by cooking, the way that it causes trouble is that it gets on your skin and in your nostrils and then causes you an infection at some unpredictable future date.
So if you are bringing raw meat with MRSA on it into your house and you are not utterly, scrupulously clean at all times, that may be a vector of MRSA entry to you or your household.
And third, it also tells us that the influence of farm use of antibiotics is more prevalent than we realize.
Q. So how should consumers respond to this?
A. What it tells me as a buyer and eater of meat is I need to be very careful about hygiene in my kitchen.
Second, as a consumer I have the ability to address the degree to which those organisms are being generated in the first place. Because, in fact, antibiotic use on [conventional] farms is causing those kinds of resistances [in both kinds of meat]. So I can use my dollars to strengthen non-antibiotic-using farms by buying their products instead of conventional ones.